Health Impacts of Climate Change: The Role of JEDI
 Introduction to the JEDI Gap
Introduction to the JEDI Gap
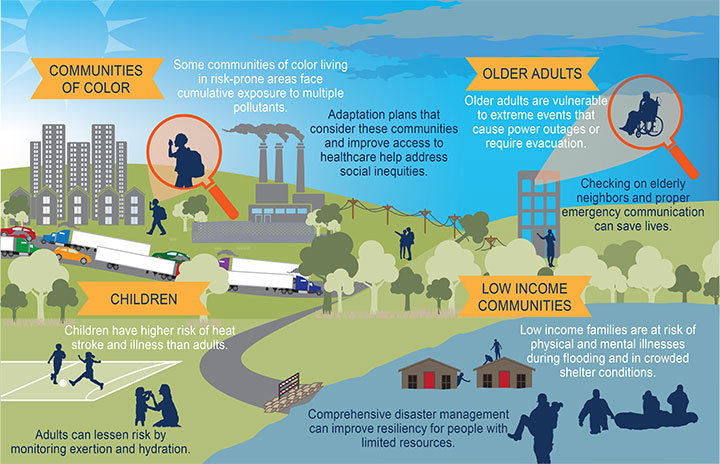
Justice, equity, diversity, and inclusion concepts are fundamental to directing resources to communities with high susceptibility to climate impacts due to historic inequities and disparities in access to a broad range of civic and private resources. Assessing the climate hazards and related threats to public health in concert with identification and prioritization of places and communities that can benefit most from adaptation building can address social determinants of health and core public health goals. Climate change impacts health differently due to a variety of personal, environmental, and social factors, such as age, location, race, and occupation. These combined factors affect an individual and community’s ability to adapt to climate-related health risks. Understanding JEDI’s role in public health is a critical step to identifying climate-sensitive populations that will be most affected by climate change. Before starting the BRACE process, it can be helpful for health departments to consider the role JEDI plays in their locality. The subsections below feature a variety of lenses through which to consider characteristics for assessing vulnerability and adaptation in a locality. While not comprehensive, the lists serve as a brainstorming tool to help health departments consider which communities and individuals in their locality are likely to benefit most from adaptation investments and interventions.
Socio-Demographic Vulnerability
The following socio-demographic characteristics increase individuals’ vulnerability to climate-related hazards:
- People with existing health conditions, especially mental illness and asthma1
- People with limited mobility2
- People with disabilities3
- People with low or no wealth
- Older adults, especially those living alone4
- Pregnant people5
- Infants and children6
- People who are linguistically or socially isolated7
- People of color, especially African Americans, Hispanics and American Indians/Alaska Natives8
Source: Fourth National Climate Assessment’s Figure 14.2 “Vulnerable Populations”